Digital transformation and simulation: NHS child health records
As populations around the world grow and live longer, healthcare organizations are seeking to digitize and automate processes to improve efficiency, drive down costs, reduce errors and deliver better patient outcomes and experiences.
Whether the Internet of Things, Big Data, Artificial Intelligence, machine learning or robotics, the availability of tools and technologies to deliver digital transformation continues to grow. A recent study by SAP Center for Business Insight, in collaboration with Oxford Economics, revealed that healthcare organizations in particular are planning to heavily invest in Big Data and analytics and cloud technologies over the next two years to help support their digitalization initiatives.
Although investment in technology is a key part to achieving success, it’s only one part of the digital transformation journey. Success depends on so much more than technology alone – it’s also important to focus on the cultural change that should go alongside technological change.
We have seen more SIMUL8 users using simulation to help plan and implement successful transformation projects. Simulation helps support cultural change by helping everyone to reach a shared understanding of current processes, as well as identifying the impact and costs of digitizing and automating processes.
A project we recently worked on with the UK NHS, looking at the automation of child health records, is a great example of using simulation to help plan for digital change.
Improving the way information about a child’s health is shared
The key aim of the NHS’ Digital Child Health Transformation Program is to promote greater use of digital tools to empower patients, enabling them to become more engaged in their health and care.
One of the outputs of this program is the implementation of new standards for electronic child health records that will allow information to be exchanged directly between different clinical and administrative systems without the need for any manual exchange. Information on screening tests, immunizations and developmental milestones from across the health system to be made available in a consistent, coherent way. They will also allow anyone involved in a child’s care, including parents, to have to a standardized set of paperless, digital child health records.
Through improved accuracy and access to information, the initiative will improve overall child health, as well as reducing the resource required to input and report on records.
Speaking about the standard, PRSB chair and GP, Professor Maureen Baker CBE, said: “Every child has the right to a healthy life and I am convinced that this new way of sharing standardized information digitally will support this goal by enabling safer and more efficient care, as well as better support for children and their families.”
How was simulation used to plan for digitization and automation?
At the start of the project, every Child Health Record Department completed a questionnaire that outlined the child population records they are responsible for, the volume of records handled, and whether records were received via email or post.
Working with a smaller group of departments, SIMUL8 Corporation and the South Central Commissioning Support Unit produced a set of process maps and recorded the average time taken for each process.
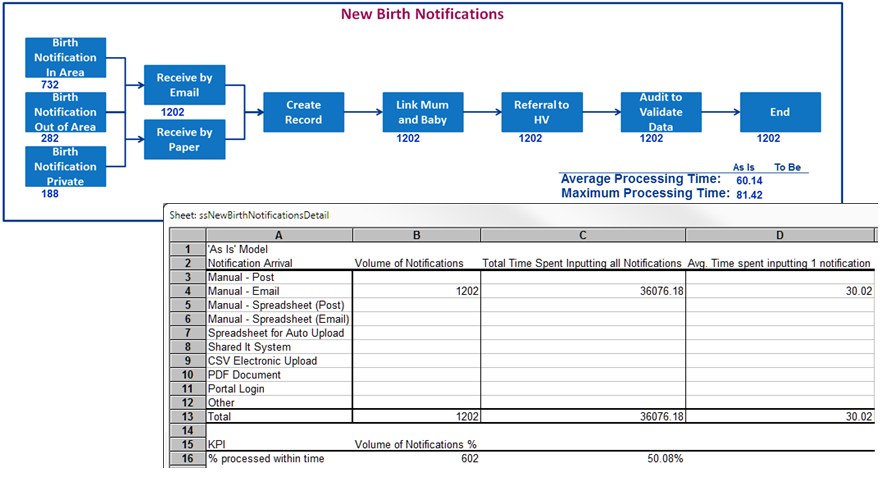
A simulation was created using the results of the questionnaires, as a series of process maps for each record. The activity in the simulation is generated by the current child population, with each process in the system triggered by the child’s age. As the simulation runs forward, each child ages one year and population projections are used to show activity volumes as a result of new births.
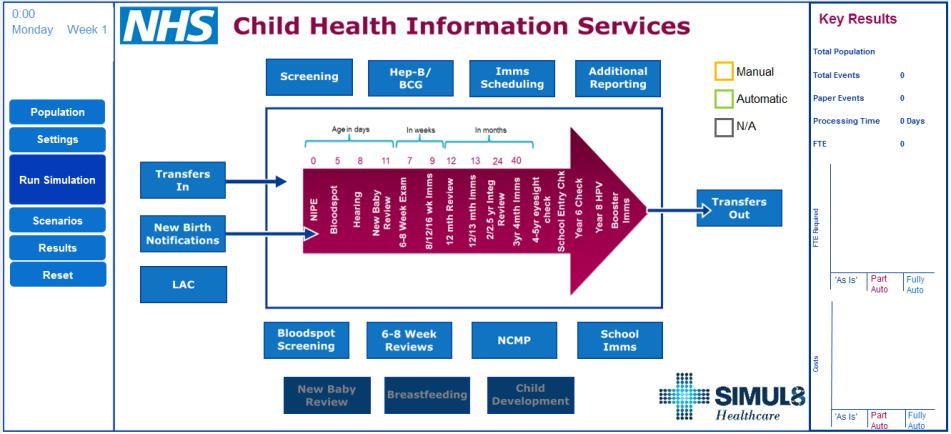
The Child Health Information Services simulation
The simulation was demonstrated to three child record departments and tested using their own populations to check the processes that had been correctly mapped and whether the resulting activity volumes accurately represented local activity. The simulation aggregated the total time taken for each process and reported the number of full time staff required to run the current service and the costs involved, to further validate the accuracy. The three departments were able to confirm that the simulation was a correct reflection of their workload. We also built in functionality to allow for local differences. For example, one department scheduled all school nurse immunizations whilst in another area this service was managed by the school nurses themselves. The simulation users could switch off any services that were not part of their workload.
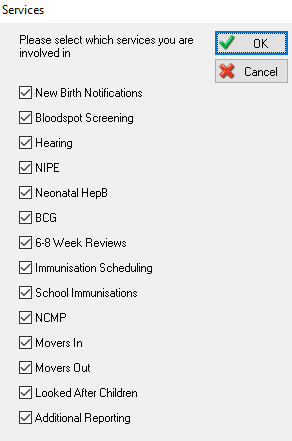
Simulation users could change the services they were involved in
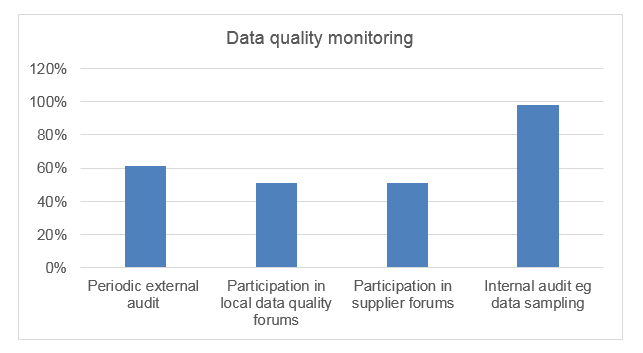
An interesting finding to come out of the mapping of the current process was seeing the amount of time spent on data quality by departments. Speaking to the staff, we found a huge commitment to ensuring that they had alerted relevant clinicians when children had not received a test, going well beyond the call of duty. We were able to report this to the national team as a key consideration for implementing the final solution, to help ensure that the ‘failsafe’ processes were robust as automation was implemented.
The next step was to build in the digital transformation scenarios in to the simulation. As the London region had already moved some way towards automating their system, we demonstrated the baseline simulation with their team lead to understand which parts of the processes were automated and which still required staff time and resource. The team also outlined the London scheme for sending text messages rather than postal letters and we included this in a ‘part-automated scenario’.
Discussing the London scenario with other departments, we became aware that there would likely be multiple part-automated scenarios depending on different local situations, and in any case, not every locality would start from the same point. We then developed a spreadsheet which listed every possible process and the time taken to complete. This could be used by localities to help test part-automated scenarios simply by setting the time associated with automated processes to zero.
Full automation of the system would not be expected to be in place for another two to three years but when fully automated, the simulation scenario sets all timings to zero other than data quality processes.
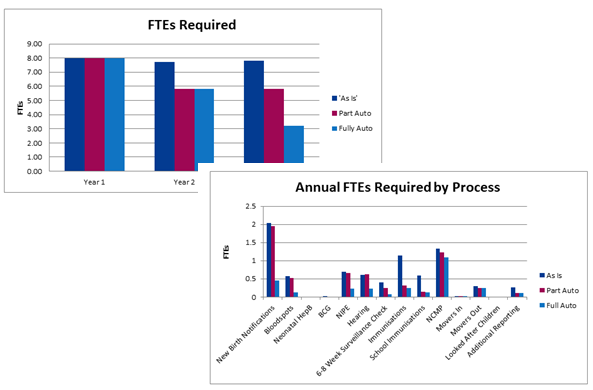
The final results of the simulation show the staffing levels that will be needed as automation is rolled out and where they should be deployed, as well as costs associated with the different automation scenarios.
As NHS England regions start to consider how to reconfigure child health information services for their local area, they are able to use the simulation to engage with their stakeholders so that all players start from a true understanding of the current process. This enables them to accurately and thoroughly test out new implementation plans for their area to gain stronger buy-in from stakeholders as they move into deployment.
This project is a great demonstration of how digital transformation will transform practice, reduce costs and deliver better, patient-centric services, as well as highlighting simulation’s key role in the planning and implementation of digital change initiatives.
Could simulation help transform your organization’s digital capabilities? Get in touch with the SIMUL8 team to discuss your goals.