Memorial Health System’s 4 steps for simulation success
Memorial Health System, a leading healthcare organization based in Illinois, have been SIMUL8 users for over five years. Simulation has supported more than 30 healthcare improvement projects across almost every aspect of the hospital system – from optimizing capacity and patient flow for a major OR expansion, to improving vehicle throughput in a hospital front drive.
In this post, Lean Six Sigma Project Manager Graham Prellwitz shares four process steps that have helped the Memorial Health System team to focus simulation projects, deliver valuable insight for stakeholders and improve patient experiences.
Want to learn more about how Memorial Health System use SIMUL8? Watch the recent webinar session, ‘Using Simulation for Facility Planning in Healthcare’ for more tips and case study examples.
Why do we use simulation at Memorial Health System?
We have seen care that is constantly transforming. A great deal of care is trending towards an outpatient environment, with free-standing emergency departments and quick clinics popping up. With this trend towards outpatient environment, we need to figure out ways to build healthcare facilities that can effectively care for those patients in a different setting than a traditional inpatient one.
We have also seen advances in healthcare technology, with telehealth, virtual visits and developments in bedside technologies. Procedures that used to have three- or five-day inpatient stays afterwards are now being completed in an outpatient environment where patients come in and go home on the same day.
We have used SIMUL8 software at Memorial for the past five years to help us plan for and meet these healthcare changes across different care environments.
Simulation has enabled us to improve patient experience throughout their entire care continuum, whether for patients who are referred to us from an outpatient clinic, or patients that are coming in through our emergency department. SIMUL8 has enabled us to better understand how those patients flow through our inpatient unit, to discharge and revisiting our system.
Ultimately, we want to leverage simulation to ensure that we are creating a process and system that is safe, efficient, repeatable and sustainable for the care that we provide and the patients that Memorial Health System serves.
To help achieve this goal, we have four key considerations to help ensure that our simulation projects meet our objectives and deliver recommendations for stakeholders.
Step 1: Know your inquiry
The first step is about knowing your inquiry and this means knowing what questions we are attempting to answer.
We have experienced great results from our SIMUL8 simulations and have made sure to publicize these to our stakeholders and demonstrate how we can utilize the software elsewhere. However, this has also resulted in people seeing simulations and getting excited thinking that they can be used to fix everybody’s issues with everything!
While it is powerful software, you need to be sure that you know exactly what questions you are attempting to answer because it will not fix every single issue that arises on an operational unit.
Save time and effort
Having awareness of a simulation’s specific purpose and goals will save time and effort for everyone involved. Those of you that have used SIMUL8 know that you can build a simple simulation in an hour or two, as well as more powerful simulations that can take longer to build as more levels of complexity are added. It’s important to make sure that you are not stretching out the process by trying to fix every single issue in a single simulation that may be better addressed in another project.
Avoid confirmation bias
Another aspect of saving time and effort is being aware of confirmation bias as we go through the process. Confirmation bias is defined as tendency to search for or interpret information in a way that confirms one’s preconceptions, leading to potential errors.
Something that we have seen is the past is that people would come to us and say “can you build this simulation, we want to build three rooms dedicated to this – can you confirm that is what we should do?”. While there are some scenarios where this approach might be appropriate – is there a purpose to building that simulation if the person making the decision already has what they want to do in mind? While it’s important to know your inquiry, we don’t want this to limit idea generation.
We want to make sure that the cornerstone of our simulations is in enabling us to explore all our options, which is why I attempt – and try to challenge everybody that I work with that builds simulations – to start with as much of a blank state as possible. Try and steer away from having a very specific outline and just going through the motions to be able to confirm someone’s assumptions. We want to try and provide other, potentially more effective options. There is a great deal of power built into SIMUL8, which allows us to explore ideas or solutions outside of the box and not just confirm what has been done in the past.
Step 2: Know your process
Conduct process mapping with stakeholders
As a Lean Six Sigma Project Manager at Memorial, I am regularly involved in process mapping when building simulations. It is really valuable to bring people together to build out an actual process map with stakeholders who work that process every day.
In healthcare, I know that that it can be difficult to pull care providers off the floor, whether due to staffing limitation issues or geographical location, but it is important to do so as we find that there can be a disconnect between what leadership thinks is happening and what is occurring.
A great deal of these issues will come out as you build a current state process map of how the space is utilized and how patients flow through that process to ensure those are accounted for within the simulation.
Ideas for improvement
Once the current state process map is completed, we start to look at future state. What opportunities have been identified as we have gone through the process mapping exercise?
This might involve considering the building of new spaces, redesigning existing spaces and making the space as efficient as possible for those that work in it. Or, it might involve launching a quality improvement initiative to dive into some issues that you might be seeing and where you think there are opportunities to improve.
Memorial Health System case study
Learn how Memorial Health System ensured the feasibility of a $31 million OR expansion project by using simulation to optimize capacity, system design, and patient flow.
Step 3: Know your space
Space utilization
Healthcare facility planning is about knowing the space that you are provided with and that you are working in, meeting with stakeholders and decision makers within your organization to determine your space utilization and looking at the physical restraints that exist that you should incorporate into your simulation.
As we build out simulations, we also want to ensure that we are looking at non-value-added spaces, such as janitorial closets, restrooms or hallways, as well as making sure that, from an organizational or accreditation standpoint, we are building simulations and giving recommendations that account for the physical restraints during the facility planning process.
Fiscal restraints and expectations
Of course, ultimately, the bottom dollar is critical. You want to make sure that you identify the fiscal restraints and expectations that are brought to you because, while you might not be the architect, you are providing recommendations and you want to ensure that they are based on realistic expectations and that the fiscal boundaries are accounted for in the simulation.
Build visualization in to your simulation
When using SIMUL8, we have found that including a background image of a floor map with animations to demonstrate people or items flowing through the simulation makes them more translatable to a wider audience.
If you have gone through and built a simulation, then you know how each of the resources and the distributions work. That being said, if your stakeholders have never been exposed to simulation before, they might not be aware exactly what is going on as things move across the screen!
We have found that once we have built the base simulation and are bringing it back to our stakeholders, adding these types of things within the simulation helps them to better understand how spaces will be utilized or how processes will work.
Step 4: Know your data
Ensure data accuracy
This is one of the most important things to know. We all know that outputs from a simulation are only as good as the inputs of data that are put in. When we collect our data, we circle back and validate it with people that work on the process, which links back to knowing your process.
A prime example that we have used in the past was when we built a simulation that looked at our emergency department and the throughputs of patients. One of the data points that we looked at was our door to doc time or how long it took once a patient came in through the door for them to be seen by a physician. When we pulled the data, we realized that there were many different definitions, depending on the person’s background of what door and what doc time was in this process.
Door might be the time from when that patient physically walks in the front door, or it could be the time from when they checked in with the triage nurse, or from when they got back to the emergency department. There were many different definitions for different data points, so going back to validate the data with the people that worked the process ensured that we were feeding good data into the simulation.
Customizing distributions
Distributions give the ability to customize the data to best represent your process. Those of you that work in healthcare know that there is a great deal of variation involved.
SIMUL8 gives you the power to build in different types of distributions to represent things like arrival rates where we might know how many patients we see on average per day or per hour, while also knowing that that can flex throughout a day or season. These distributions can be used to make a more powerful and accurate simulation that takes this variation into account.
Data checklist
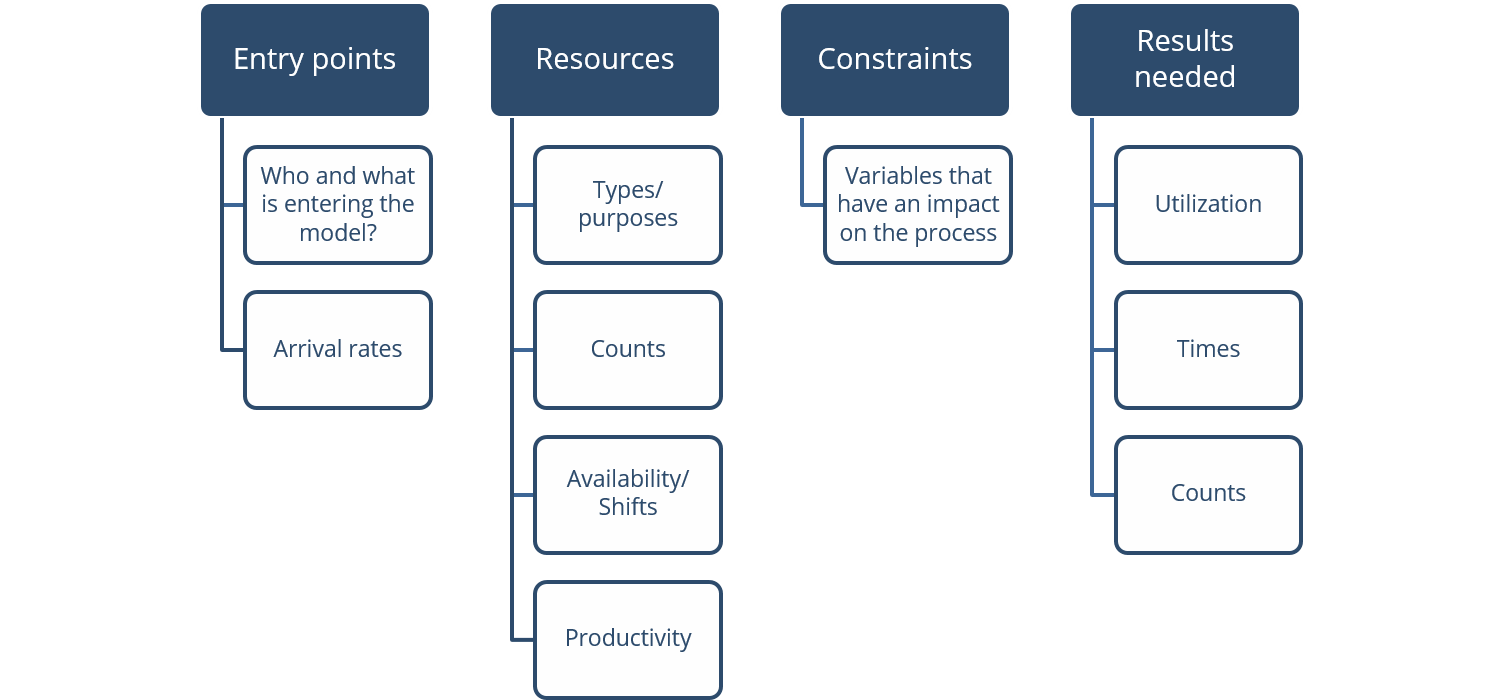
As we look at the data that we want to bring in, this is a checklist that I use to break down data into four points.
- Entry points – who and what is entering the simulation and at what rate?
- Resources – what type of resources do we have available and how many do we have of each? Availability, shifts and productivity is something that we see a great deal as we build these new spaces, while looking at our staffing schedules and where opportunities might be available to help elevate clinical care takers to be able to work at the top of their license.
- Constraints – what are the queuing times or other variables that might have an impact on process come to light as we go through and build the process maps to identify constraints?
- Results needed – what information do we need to make informed decisions? This also comes back to knowing your inquiry and what you are looking at. It could be room utilization, turnaround times for rooms after patient discharge, counts or volumes as patients move through.
We have found that if we can answer the questions in these four points, we can build more effective simulations. Our planning team can then use these recommendations to build out the space or process to create an efficient and effective area for care for our patients.
How have these points been applied to real projects?
In our next blog posts, we’ll look at how these four considerations have been applied to two real healthcare facility planning projects at Memorial Health System – one to improve vehicle throughput in the front circle drive at their 500-bed flagship hospital in Springfield and the other to rebuild a portion of a small critical-access hospital to centralize five different testing areas.
Learn more about SIMUL8 for healthcare
Build a business case for healthcare process change, reduce costs and improve patient care using simulation.
