10 challenges healthcare providers can overcome using simulation
The continued uncertainty facing the healthcare industry in 2018 and beyond is leading organizations around the globe to improve efficiency across every function. As a result, more healthcare providers are turning to simulation to help them find, plan and implement improvements.
Why? Simulation allows you to solve problems and thoroughly test any changes to healthcare processes in a risk-free, virtual environment. You can simulate almost anything anything – from the flow of patients through an emergency department, to the staff schedule for an inpatient unit or call center, or the day-to-day operations of the central sterile department.
Every healthcare system has its own unique set of challenges, but there are still many common obstacles and issues faced across the whole industry. In this blog post, we’ll look at how simulation is helping organizations to overcome these key challenges without risk to patients, staff or financial investment.
Download the ebook: Download the ‘Top 10 Impacts of Simulation in Healthcare’ ebook version of this blog article
1. Understand where variation occurs and the impact it has on services
Every day is different in healthcare. Patients have different needs, they will arrive at different times and demand for services changes throughout the weeks, months and years. This variation creates an uneven demand on services, so it’s critical to know what resources you need to have in place, at the right time, to ensure a smooth flow of patients and minimize delays to their assessment and treatment.
Traditional approaches like spreadsheet models based on fixed values can make capturing this variation difficult, if not impossible. With simulation, you can accurately model variation to really understand why your system behaves the way it does. You can also test any number of “what if?” scenarios to make better, more accurate decisions around approaches for managing variation and ensuring you have the appropriate resources in place.
2. Ensure effective use of healthcare resources
Whether your resources are beds, staff or equipment, you will always have questions about how they should be most effectively deployed to meet patient needs, minimize waiting and reduce waste.
Simulating varying demand and constraining it by the resources you have available provides the evidence you need to meet waiting time targets, better utilize existing assets or even to make stronger business cases for investment in more resources.
“You can say, ‘What happens if I increase my person load coming to the ED by 20%?’. You can plug that into SIMUL8 and ask what that would do to the resources and how many LWOTs there would be, or what the efficiency would be of staff and whether we would be burning them out.”
Raul Medina, Lean Six Sigma Black Belt and Lead Process Improvement Coordinator
SIMUL8 case study example: Learn how Vidant Duplin Hospital maintained ‘left without treatment’ rates with increasing patient volumes using simulation and Lean Six Sigma techniques
3. Reducing handoffs
Many healthcare errors or delays can be traced back to problems at handoffs – parts of a process that involves the transfer of patients from one healthcare setting to another.
Simulation can be used to identify where disconnects in current processes exist, as well as testing system changes in a risk-free environment to improve the flow of patients and minimize the impact of adverse events.
NHS 24, a UK healthcare call center service, used simulation to test the most efficient way of managing busy periods. When an urgent call is received, it is answered by an initial call handler, who passes the call to the ambulance service or a nurse adviser. If no nurse adviser is available, arrangements are made for one to call back within a certain period. This ‘call back’ process resulted in some patients waiting more than an hour to be called back at peak times.
Using simulation software to test improvements enabled NHS 24 to quantify the most appropriate resource and skills mix, identify the level of demand that could be handled by all stages in the process, and reduce reliance on ‘call backs’.
SIMUL8 case study example: Learn how simulation provided an accurate means for NHS 24 to test the benefit of proposals in advance of implementation, avoiding potential costly errors in design
4. Evaluate the impact of change over time
In most healthcare processes, patients are diagnosed with a condition and visit a healthcare provider for treatment. If they need a series of treatments, the patient will return at regular intervals to complete their care. Calculating the cost of this process using a spreadsheet methodology might look something like this:
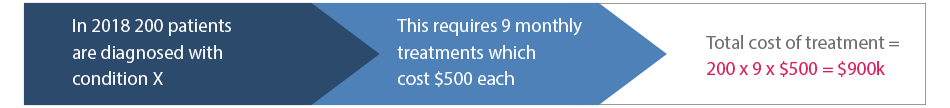
But does this actually match reality? Patient 1 could be diagnosed in April, and patient 105 in October. Patient 1 will complete their treatment in 2018 and patient 105, and all other patients diagnosed after them, won’t complete treatment until the financial year 2019-20. In some cases this might be further complicated if some patients aren’t well enough for treatment and need to be recalled later.
Simulation enables you to take into account the passing of time, as well as the individual patient complications that can delay treatments, to produce a more accurate prediction of future activity, cost and resource requirements.
Time to diagnosis was a crucial factor in Shout It Now’s work in HIV and Aids in South Africa. The charity set up pop-up street diagnostic clinics with the aim of providing quick diagnostics and counseling to young South Africans. They were able to simulate the diagnostics process to ensure minimum delays, doubling the number of people diagnosed and ensuring that 95% of those diagnosed would go on to receive treatment.
SIMUL8 case study example: Learn more about how SIMUL8 simulation software supported Shout It Now to help improve HIV screening and treatment
5. Identifying bottlenecks in a complex environment
When there are long waits in a healthcare system, how can you identify the best way to improve the situation? With so many external and internal factors to consider, it can be challenging to really know where and what to improve to make the biggest impact. Factors that will make the biggest difference could require a long negotiated lead time with multiple organizations, while others could be quickly implemented and make an immediate, if smaller, difference.
Simulation can help you to quickly pinpoint these issues – for example, is it a lack of emergency medicine physicians, a lack of beds, or community facilities for discharge that is the problem? You can then use the simulation to test improvement scenarios and demonstrate which will be most effective.
For example, a hospital used simulation to test several improvements to try and reduce emergency admissions and readmissions:
- Focus on support for care homes
- Increased primary care services
- Increased ambulatory care
- Increased ambulance ‘see and treat’ services
They also tested the impact of each scenario in the light of an increasing population over the next few years to understand the long-term consequences. Out of all these options increasing ambulatory care had the biggest impact on admissions. With demand at current levels, this would mean that inpatient beds could be reduced by between 20 and 50 depending on the scenario selected.
“With ongoing cost reductions and other restrictions within the healthcare environment, clearly our resources are getting to be very precious and scarce, so we need to use tools like SIMUL8 to make sure we are getting the highest performance we can get out of the most reasonable amount of resources.”
Jim Scheulen, Chief Administrative Officer, Johns Hopkins
SIMUL8 case study example: Learn how Johns Hopkins Health System have used simulation software to optimize ED patient flow, reduce waiting times and empower strategic decision making
6. Improving population health and reducing obesity
Planning for the health of a population is crucial to ensure the best outcomes, effectively manage demand and ensure quality services.
Simulation can be used to understand the impact of key population health issues and support healthcare networks to achieve the quality of care, cost and better population health.
As people move through a pathway of care, the likely outcomes can be modeled at each stage over time to enable effective prediction of services and costs on an annual basis.
For example, obesity is a growing issue that is having a serious impact on the health outcomes of populations around the globe. Interventions to reduce the trend include public health and lifestyle, as well as clinical interventions shown in the four tiers here.
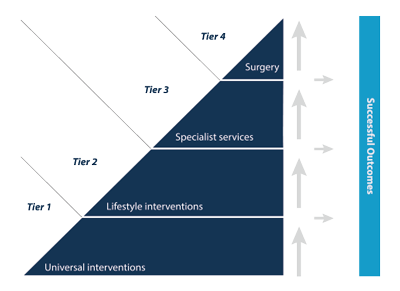
Using simulation, they could predict how long patients would stay in each tier and therefore how many would need a service and the length of stay in that service. In turn, the simulation results provided evidence to commission obesity and weight management services with confidence.
SIMUL8 resource: Learn more about how simulation helps healthcare organizations to understand and plan for population health issues
7. Supporting patients in ‘out of hospital’ settings
In planning services from a population perspective, as an Accountable Care Organization does, the first thing to understand is how the population currently uses services and how that might change in the future. Analysis of your population against service utilization will enable you to identify patient groups and how they behave, and help guide discussions on how and where in the healthcare system interventions should be made.
Simulation can predict the demand on the system as the population ages using population projections. Patients follow different pathways through the system depending on their needs and these can be simulated as a dynamic process flow, costing each part of the service and showing any bottlenecks as the simulation runs over time.
For example, a healthcare provider wanted to evaluate whether introducing a night nursing service would reduce emergency admissions for people who could have been cared for at home.
By creating a simulation, the ‘before’ scenario demonstrated how patients currently use services and an ‘after’ scenario showed the impact of night nursing as well as the additional capacity required to meet need. The project used simulation to show stakeholders how effective the new service was, and provided operational evidence for financial decision-making about the most effective interventions to fund.
8. Managing care for people with long-term conditions
As our population gets older, more people are living with chronic disease. Research demonstrates that those aged over 65 are also more likely to have more than one long term condition.
Health services tend to plan care by specialty, but what if this changed to a person-centric care model? Would it result in a reduction in hospital visits and costs, or would it fund more community based support whilst hospital costs stay the same? As the population ages, and this group increases, will there be enough community nurses to support people outside hospital?
NHS England has been encouraging pilots of this approach to care for some time. A recent successful model of extensivist care from Fylde Coast has been adopted by using local data in the simulation to test the impact of implementation.
In their simulation, target patients in a health system are identified through risk stratified profiling. Users can segment the population into groups representing different types. Some choose to group people by numbers of long term conditions, others include further characteristics such as whether the person lives in a residential care setting. Each group has a different probability of accessing a service during the year, and the full range of services is included: primary and community, hospital and acute, mental health, social care. A frequency probability is applied so that each person may access a service multiple times, and a cost and a resource linked to each service.
The simulation transitions people between the groups as their conditions change. The simulation runs forward over a number of years from the current state and results predict the annual cost of service by person and category of service for each group and the numbers of staff, beds or other resource required. Cost and capacity requirements are also shown for each year to help support planning decisions. Simulation users can also experiment with the new models of care they wish to implement and can test the impact of these on cost and capacity.
The simulation is used as a way of disseminating new models of care, and allows others to experiment with the impact of adopting them in their area. It allows change to be implemented over time to understand the cost of the new model of care against the likely savings from reducing hospital admissions and whether this is an affordable option over time.
SIMUL8 resource: Download our ebook to learn how NHS England is using simulation to adopt new models of patient centred care
9. Reconfiguring services without risk
Drives for efficiency and merging of healthcare organizations often result in a restructuring of services. Simulation can help planning for the restructure to ensure that demand can be catered for without delay, staff and facilities are available, and procedures scheduled to make the most efficient use of resources.
Memorial Health System simulated the design of a new state-of-the-art $31m OR suite, expanding to 22 ORs to meet a 3-5% annual increase in surgeries. They used simulation to identify any process bottlenecks and found that the two elevators originally planned in the design would delay transportation of patients and increase cancellations. The additional cost of another elevator when compared with the loss of revenue meant that it would pay for itself in just a few weeks!
“SIMUL8 has been a valuable application for expanding our range and depth of analytical abilities. It should be considered an important tool in the design of every robust healthcare performance improvement program.”
Todd S. Roberts MBA, System Director of Operations Improvement, Memorial Health System
SIMUL8 case study: Learn more about how Memorial Health System ensured the feasibility of their OR expansion project by using simulation to optimize capacity, system design, and patient flow
10. How many hospital and community beds do you need?
Managing bed capacity is key to the smooth running of a hospital since all departments are in some way dependent on bed availability. As well as improving patient flow and outcomes, better bed management has been shown to save as much as $370,000 per month per hospital.
However, many hospital planners still rely on deterministic spreadsheets, based on average demand, to plan and manage their bed capacity. Without considering variation in demand, it could look like there are enough beds. But in reality, patients regularly have to be placed in a non-ideal unit when beds are unavailable, or have to wait in the emergency department until a bed becomes available.
Simulation enables you to mimic the flow of patients through hospital wards and produces results which show at what point in time patients are unlikely to get a bed in their specialty area, and the impact on waiting times.
NHS Isle of Wight used simulation to create a replica of emergency and elective demand and bed capacity by specialty on an hourly basis over a year. Their results revealed that in some specialties they were over capacity for elective demand and under capacity for emergency demand. By demonstrating these results to staff and commissioners, they were able to get buy-in for changing the use of beds, gaining 17% additional capacity for medical inpatients within their existing bed base.
SIMUL8 case study: Learn more about how Isle of Wight NHS Trust improved bed management and planning using simulation
Learn more about using simulation for improving healthcare processes
No matter your specific challenges, simulation enables healthcare systems and processes to be tested in a safe, virtual environment without risk to patients and staff – supporting organizations to make better decisions, improve systems of care and maximize resources.